From infection prevention to telemedicine, the COVID-19 pandemic dramatically changed health care access and delivery. As hospitals looked to reserve beds, resources and staff for COVID-19 surges, patients embraced staying at home. They opted for more remote health care, including options for care that otherwise would only have been available within a hospital.
Although telemedicine is far from new—a version was conducted over the telegraph as far back as the 1800s—it did not become ubiquitous until the COVID-19 pandemic, she says.
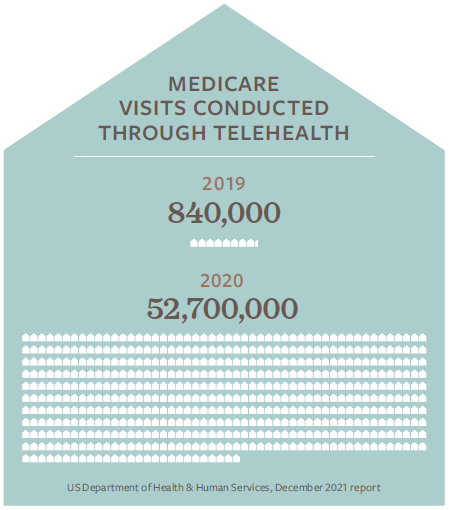
The share of Medicare visits conducted through telehealth, skyrocketed from approximately 840,000 in 2019 to 52.7 million in 2020, according to a December 2021 report from the US Department of Health & Human Services.
Not only did shelter at home orders make home care a more attractive choice, but access to (and reimbursement for) telehealth services was expanded.
“I think anytime we can facilitate a patient being more comfortable and still having the same safety and monitoring [as in a hospital], we’re doing them a service.”
DR. SARAH PLETCHER
SYSTEM VICE PRESIDENT AND EXECUTIVE MEDICAL DIRECTOR OF STRATEGIC INNOVATION AT HOUSTON METHODIST

In March 2020, the Centers for Medicare & Medicaid Services (CMS) used emergency waiver authorities to implement the Hospitals Without Walls program. Later, CMS followed up with its Acute Hospital Care at Home waiver program, which allows eligible hospitals to treat patients at home for services traditionally provided in acute care hospitals.
CMS has stated that treatment for more than 60 different conditions, such as asthma, congestive heart failure, pneumonia, and chronic obstructive pulmonary disease (COPD) care, can be treated at home with proper monitoring and treatment protocols.
Some patients with COVID-19 or those who need a medication like IV antibiotics may also do well with virtual care if they are monitored effectively, says Pletcher. As well, patients with cognitive issues tend to have better outcomes at home than in a busy hospital environment, she adds.
Technology Enables Providers to Up Their Game
Innovations like remote technology, which allows care providers to collect data from the patient in the home setting, are helping Texas hospitals make home health care more viable. For instance, Houston Methodist, has partnered with the technology company BioIntelliSense to provide medical-grade remote monitoring and analytics technologies for in-hospital and at-home patients. This technology allows doctors to measure up to 1,440 sets of vital sign measurements per day on patients who wear BioButtons or BioStickers.
“This [partnership] becomes really a game changer in terms of just putting a sticker on a patient and having data insight about where we need to adjust our treatment plan,” Pletcher shares. Patients need to rest and recover instead of being woken up every eight hours to have their vital signs checked, she adds, calling this approach “antiquated.”
Hospitals and home health care agencies have also joined forces to help make hospital-grade home health a reality. Memorial Hermann Health System, for instance, recently partnered with home care provider Contessa, an Amedisys company.

Similarly, CHRISTUS Health, a Catholic not-for-profit system made up of more than 600 centers (including about 60 hospitals) and the home health, hospice and long-term acute-care provider LHC Group began a joint-venture partnership back in 2017. Although the partnership initially focused on delivering traditional home health, once the pandemic started “raging,” the partners “doubled down” to provide remote care, especially for chronic care patients, who often ended up in the Emergency Department, says Michael Talley, vice president of clinical operations for CHRISTUS Health.
From Talley’s perspective, the beauty of the collaboration is that CHRISTUS doesn’t have to duplicate LHC Group’s services and that it can draw on better economies of scale. “We can’t do it all on our own–we don’t have the dollars, the infrastructure or the know how that LHC has.” Another benefit is that home health care can help address unnecessary days in the hospital beyond the resolution of a patients acute medical needs. These additional days are often due to a lack of resources or “a litany of other social reasons,” says Talley. For example, CHRISTUS can cover the cost of home health on behalf of uninsured patients, which enables nurses to free up hospital beds for patients who are critically ill.
“This speaks directly to my heart. I know for myself, as a past caregiver, you want to see the patients who need you the most and you don’t want to turn away folks in need because you have someone else in a bed who may be better served in a different care environment.”
MICHAEL TALLEY
VICE PRESIDENT OF CLINICAL OPERATIONS FOR CHRISTUS HEALTH
In addition to providing patients a more convenient and comfortable health care option, virtual care can also be used as a retention strategy for associates. “We’re in a new era where you now have another alternative for nurses who are nearing retirement, or who are afraid to be at the bedside anymore due to the pandemic,” says Talley.
Home Health Care Barriers
Although digital tools and virtual health care are on the rise, they are not a replacement for traditional care options. As Pletcher points out, home health cannot always provide the same level of sophisticated and complex care provided in a hospital as there are still barriers in terms of coordinating medical equipment.
“Do they need a hospital bed, do they need oxygen, do they need an IV? Do they need a ramp in the home?” she asks. Care providers also must think about how they’re going to “air-traffic control” all of these things — who is going to go to the house each day to give the patient the necessary care and what is the wrap-around command center software that will help them manage information, she says.

“We recognize that having a recovering hospital-level patient in the home environment isn’t for every patient and isn’t for every family.” For instance, it may not serve a fragile, mobility-limited patient living with an overwhelmed elderly spouse or a patient who shares accommodation and wants a more private hospital setting, she says. She also points out that not every house has reliable heating or cooling systems.
Additionally, some seniors are not savvy with technology, which can interfere with the delivery of virtual health care, says Loomis. According to a 2020 report from Aging Connected, a nationwide campaign to get seniors better connected, 42 percent of older Americans lack adequate broadband access. Furthermore, some patients in remote areas do not have access to Wi-Fi and patients with limited resources may not have access to a smartphone, adds Talley.
During the 2021 legislative session, THA supported two key bills to help expand access to telemedicine and telehealth services across the state. Longtime advocate for telemedicine issues, Rep. Four Price (R-Amarillo) passed a bill to make permanent the telemedicine flexibilities that were put in place during the pandemic to ensure access to care for Medicaid and CHIP clients. Rep. Trent Ashby (R-Lufkin) also passed a bill that expands access to reliable broadband internet services to support access to telemedicine.
Changes in Reimbursement
Although the CHRISTUS-LHC partnership did not delve into virtual health until 2020, in 2017, the partners did initiate a remote patient monitoring program in Texarkana that helped reduce the rates of hospital readmissions significantly. Despite its success, the program was at risk of shutting down once grant funds ended as there was no reimbursement for virtual care at the time.
After the public health emergency (PHE) was first declared in January 2020, Medicare relaxed the rules governing telehealth so that patients could receive visits at home as well as a wider array of services via telehealth. These flexibilities will end for most beneficiaries after the PHE ends, likely on Oct. 13, 2022. “We’re now constantly monitoring how far the public health emergency will be extended and what is or isn’t being reimbursed in this ever-changing environment,” points out Talley.

Jennifer Elder, director of regulatory affairs for the Texas Association for Home Care & Hospice (TAHC&H), notes that Texas House Bill 4 has made certain State COVID-19 flexibilities, such as the delivery of physical therapy or occupational therapy via telehealth, permanent for Medicaid Providers. As well, this summer, TMHP released the Telemedicine and Telehealth Benefit Information to Be Updated September 1, 2022 notice which details additional information related to telecommunications.
Before the pandemic, home health providers saw a funding gap of an estimated 17% in terms of allowable Medicaid costs, a gap made worse by the increasing costs of gas, PPEs, workforce costs and COVID-19-related infection control procedures, says Jessica Boston, TAHC&H director of government affairs.

The TACH&H advocates for rate increases as well as for legislation, such as the Choose Home Care Act, Preserving Access to Home Health Act and the Home Health Emergency Access to Telehealth (HEAT) Act, which will expand care choices for Medicare beneficiaries post- hospitalization. The HEAT Act will also allow home health providers to care for patients via telehealth when appropriate.
For her part, Pletcher says there have been great strides in reimbursement parity in waiver programs because payors are interested in encouraging hospitals and health systems to best figure it out. “We are still learning how to best do that and which patients are appropriate and which are not,” she says, adding that some of those reimbursement programs are meant to encourage innovation in order to see what’s possible.