Mental health concerns touch everyone across the U.S., whether a person struggles with it themselves or knows someone who does. But Texas is one place where the needs are particularly acute.
Swaths of the state lack reasonable access to behavioral health professionals and services, and according to UTHealth, Texas ranks last in the nation in youth access to mental health care. Significant gaps in payer coverage for both children and adults exacerbate the problem.
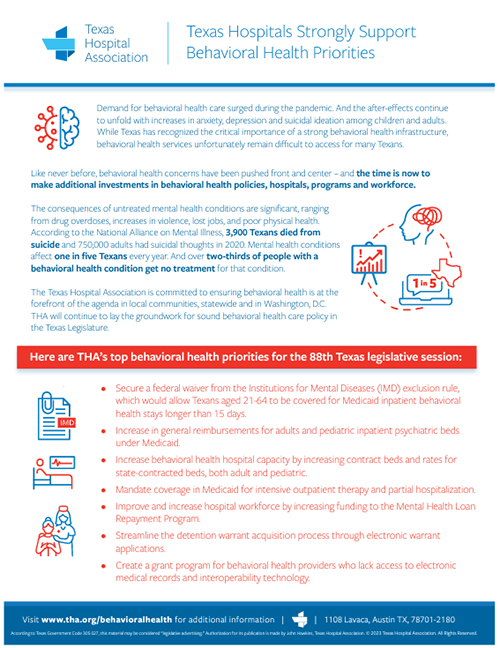
Behavioral health is a perennial priority for THA, and the 2025 session of the Texas Legislature will once again feature Texas hospitals making a push for progress.
The Issue
Data abound showing that Texas is in the midst of a mental health crisis – and that access to care for behavioral health conditions is well short of the state’s need:
- An analysis conducted in February 2023 showed 36.8% of Texas adults reported symptoms of anxiety and/or depressive disorder, higher than the national average of 32.3%.
- Youth behavioral health data show that 17% of Texas children under 18 report having an emotional, mental, developmental, or behavioral health problem, and one in three Texas children experience a mental health disorder in a given year.
- Texas has about 10 child and adolescent psychiatrists per 100,000 children, well short of the needed 47 per 100,000.
THA’s efforts on behavioral health in 2025 will be largely focused on closing gaps in coverage and promoting access to a full continuum of services just like patients receive in physical care.
The Steps in Between: Partial Hospitalization, Intensive Outpatient Therapy
For behavioral health patients in Texas’ large and vulnerable Medicaid population, there are usually two types of care: round-the-clock inpatient stays and outpatient treatment. The continuum of care between those two options – a staple of physical care – is virtually nonexistent.
Coverage of partial hospitalization programs (PHP) and intensive outpatient therapy (IOT) would provide patients with options for intermediate steps. PHP allows patients to receive behavioral health services during the day and return home at night, instead of being confined during an inpatient stint. IOT is a diverse group of intermediate-level treatment options that offer patients more flexibility and more care traditional outpatient therapy. These programs are typically only a few hours per day, three to four days per week.
THA supports required coverage for both partial hospitalization programs and intensive outpatient therapy in Medicaid.
A Barrier to Inpatient Care: The IMD Exclusion
Adult inpatient mental health care in Medicaid is capped – and hampered – by a long-standing limit on care in “institutions of mental disease,” (IMD), essentially defined as mental health facilities with more than 16 beds.
Under the IMD exclusion, Medicaid inpatient stays for patients ages 21 to 64 are limited to just 15 days of coverage. However, federal policy in effect since 2018 allows states to pursue a waiver from the IMD exclusion and allow for longer inpatient stays.
THA supports legislation and necessary funding for Texas to pursue an IMD exclusion waiver.
Building on Gains: 2023 Accomplishments
In 2025, THA will remain focused on policies that grow the continuum of behavioral health care and increase access to care for all Texans with behavioral health needs, emphasizing budget and policy items that further build on recent progress.
The current biennial state budget, crafted by the Legislature in 2023, featured key steps forward in funding that Texas hospitals greatly appreciated, including:
- A 1,300% increase in funding for the Loan Repayment Program for Mental Health Professionals, which incentivizes practicing in a Mental Health Professional Shortage Area.
- $200 million to maintain and bolster psychiatric bed capacity in both rural and urban areas, which included almost 200 new state-purchased beds.
- $16 million for a grant program to construct inpatient mental health beds at children’s hospitals.
- $7.4 million for telepsychiatry consultations for rural hospitals.
Resources
- Texas Hospitals Strongly Support Behavioral Health Priorities (THA white paper for 2023 legislative session)
- Improve Access to Mental Health Treatment With an IMD Exclusion Waiver (THA white paper)
- The State of Mental Health & Behavioral Health in Young Texans (Every Texan, 2023)
- Child Behavioral Health report (UTHealth, January 2023)
THA Behavioral Health Council
Charge: To discuss and make policy recommendations to the Council on Policy Development regarding behavioral health care issues affecting hospital members that provide behavioral health services (meets as needed).
MEMBERS
Chair: Mandy Westerman, LCSW, Kingwood Pines Hospital
Vice Chair: Zelia Baugh, JPS Health Network, Fort Worth
Aleen Arabit, San Antonio Behavioral Healthcare Hospital
Christine (Chris) Bryan, Clarity Child Guidance Center, San Antonio
Heather Chung, Ph.D, Houston Methodist Hospital
Sally E. Taylor, MD, University Health, San Antonio
Sherry L. Cusumano, RN, Medical City Green Oaks, Dallas
Christopher R. Dowers, Westpark Springs, Richmond
Kathy Griffis, Titus Regional Medical Center, Mount Pleasant
Charlzetta (Charlie) McMurray-Horton, Ben Taub General Hospital – Harris Health System, Houston
Stephen M. (Steve) Glazier, FACHE, UT Harris County Psychiatric Center, Houston
Edgar E. Prettyman, Psy.D, Texas NeuroRehab Center, Austin
Becky Tresnicky, Valley Baptist Medical Center – Brownsville
Staff Representative: Sara González, Texas Hospital Association, Austin
Related Articles
Texas Needs More Behavioral Health Care Strides in 2025
The impact of behavioral health confronts us all, whether it’s…
Taking Stock: The 2023 Regular Session
THA staff looks back at wins and challenges in member…
Pursuits of the Mind
THA is spending Mental Health Awareness Month seeking advancement on…
Closing the Mental Health Gap
Medicaid IMD Exclusion on the move in budget talks, offering…